Let’s have an open conversation about something many women experience but don’t always talk about—fibroids. These common growths in the uterus can affect your health and well-being in ways you might not even realize. At Srinivas Priya Hospital, we’re all about women’s health, so let’s dive into the basics and clear up some of the mystery surrounding fibroids.
What Exactly Are Fibroids?
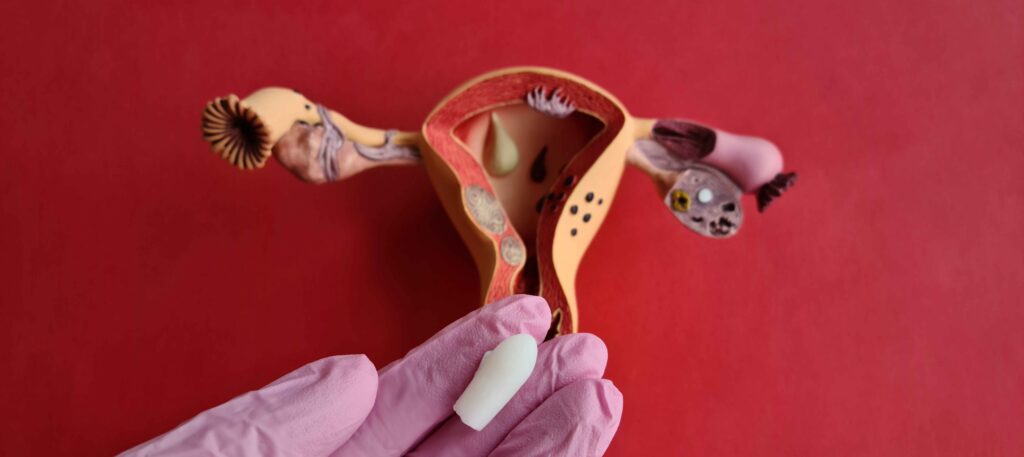
First things first—fibroids are non-cancerous growths that form in or around the uterus. They’re made up of muscle and connective tissue, and they can show up in different places. For example
- Inside the uterine wall (intramural fibroids)
- Under the uterine lining (submucosal fibroids)
- On the outer surface of the uterus (subserosal fibroids)
- Or attached by a little stalk (pedunculated fibroids)
Fibroids can be tiny or grow big enough to cause noticeable symptoms. Every woman’s experience is unique!
Age : As you age, your risk of breast cancer increases. Most breast cancer diagnoses occur in women over 50.
Family History : If you have close relatives—such as a mother, sister, or daughter—who have been diagnosed with breast cancer, especially at an early age, your risk is higher.
Genetics : Certain inherited gene mutations, most commonly BRCA1 and BRCA2, significantly raise the risk of breast cancer.
Menstrual History : Women who began menstruating before age 12 or experienced menopause after 55 have a slightly higher risk due to prolonged oestrogen exposure.
Previous Breast Conditions : If you’ve been diagnosed with atypical ductal hyperplasia or lobular carcinoma in situ (LCIS), conditions that affect breast tissue, your chances of developing breast cancer increase.
Gender : Breast cancer primarily affects women, though men can also develop the disease.
2. Modifiable Risk Factors
These are factors within your control. By making certain lifestyle changes, you can lower your risk of developing breast cancer.
Alcohol Consumption : Women who consume more than one alcoholic drink per day have a higher risk of developing breast cancer. Limiting or avoiding alcohol can reduce your risk.
Obesity and Weight Gain :Postmenopausal women who are overweight or obese have a higher chance of developing breast cancer. Maintaining a healthy weight through diet and exercise can lower your risk.
Lack of Physical Activity : Regular exercise helps maintain a healthy weight and balances hormones, both of which can reduce your risk.
Hormone Replacement Therapy (HRT): Long-term use of combined hormone replacement therapy (oestrogen and progesterone) during menopause increases the risk of breast cancer. Talk to your doctor about alternatives or the shortest possible duration of use.
Smoking : There is growing evidence linking smoking to an increased risk of breast cancer, particularly in premenopausal women. Quitting smoking offers many health benefits, including a lower risk of breast cancer.
Early Detection and Screening
Even if you have multiple risk factors, it doesn’t mean you’ll necessarily develop breast cancer. It just means you should be vigilant about screening and early detection. This can make a huge difference in outcomes.
So, what can you do to detect breast cancer early?
There are two ways to detect breast cancer eraly. They are:
Mammograms : A mammogram is an X-ray of the breast and is one of the most effective tools for detecting breast cancer early, often before any symptoms appear. Women should begin regular mammograms at age 40, but those with a family history of breast cancer may need to start earlier. Talk to your doctor about the best screening schedule for you.
Breast Self-Exams : Regular self-exams can help you become familiar with how your breasts normally look and feel. If you notice any changes such as lumps, nipple discharge, or skin changes, consult a doctor immediately.
